Unveiling the Link Between quantitative EEG and Slumber Disorder Patterns for Enhanced Diagnosis and Therapy
Slumber apnea is a common sleep condition that affects many individuals throughout the globe. It happens when a individual's respiration is disrupted during slumber, resulting to subpar slumber standards and multiple medical concerns. One of the methods scientists and physicians are working to better understand and diagnose sleep apnea is through a method called quantitative EEG, or qEEG. This approach measures the electronic function of the cerebrum and can offer valuable understandings into how sleep apnea affects brain activity and general health.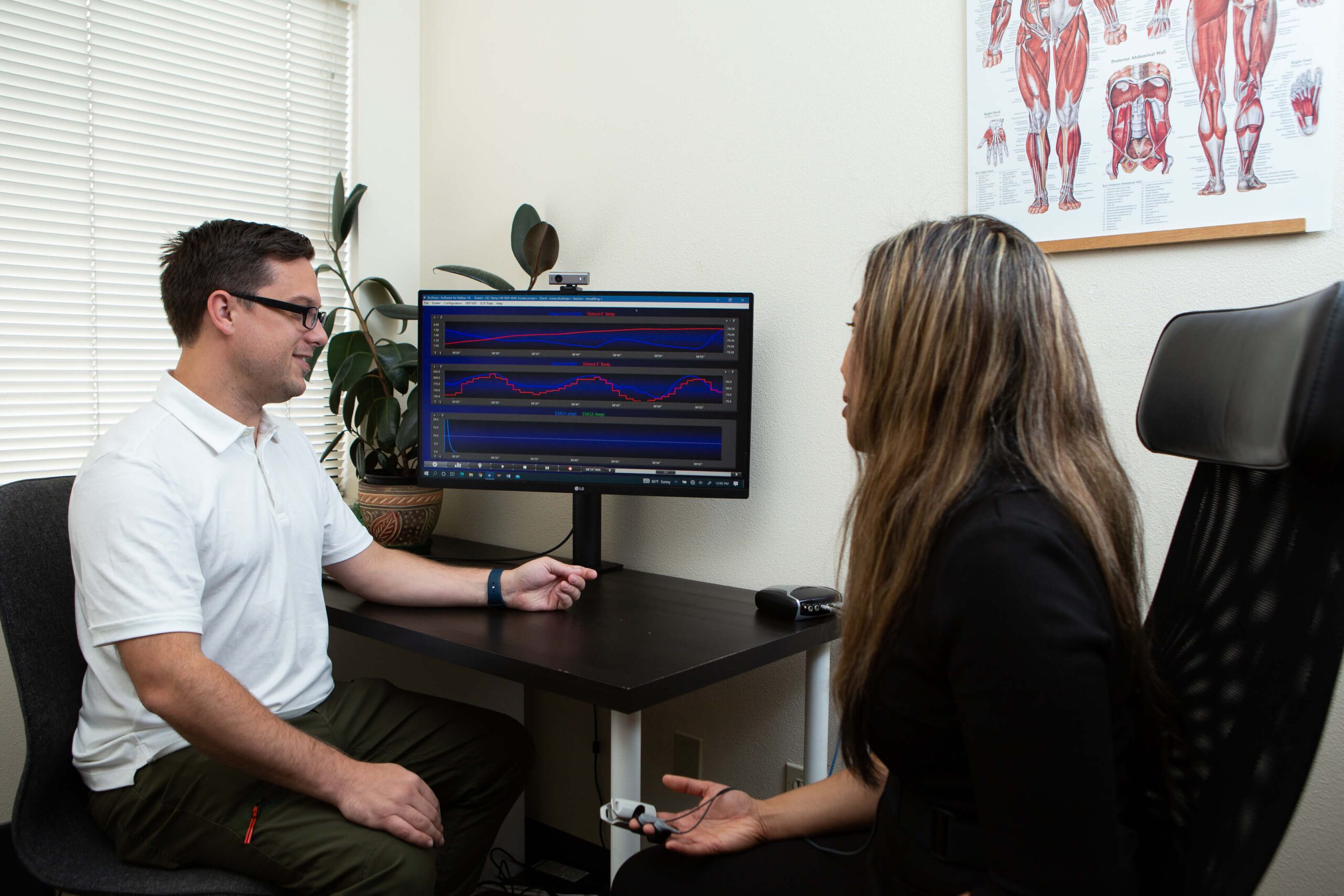
qEEG entails placing small sensors on the scalp to record brain waves. These brain oscillations are then examined to detect patterns that may indicate sleep disorders, including sleep apnea. By examining these trends, healthcare providers can gain a more precise picture of how sleep apnea disrupts normal cerebral activity during slumber. This information can be crucial for formulating effective therapeutic plans customized to individual patients. Understanding the relationship between qEEG and sleep apnea can lead to enhanced diagnostic techniques and better outcomes for those affected by this condition.
Studies has demonstrated that individuals with sleep apnea often exhibit specific changes in their cerebral oscillation patterns. For instance, during episodes of apnea, the sleep disorder diagnostic criteria cerebrum may exhibit increased activity in specific areas while other regions become more active. These changes can influence how effectively a individual slumbers and how refreshed they perceive upon waking. By employing qEEG to monitor these brain oscillation patterns, physicians can identify particular traits of sleep apnea in clients, which can assist in formulating a more precise diagnosis. This is particularly crucial because sleep apnea can sometimes be confused for other sleep conditions, leading to misguided therapies.
In addition to enhancing identification, qEEG can also play a role in assessing the efficacy of therapies for sleep apnea. For example, after a client starts using a continuous beneficial airway pressure (CPAP) machine, which helps maintain the airway open during slumber, qEEG can be used to evaluate alterations in brain function. If the cerebrum shows enhanced patterns of slumber after starting treatment, it may suggest that the treatment is functioning effectively. This feedback can assist physicians make necessary adjustments to treatment strategies, guaranteeing that clients receive the best treatment feasible.
Overall, the connection between qEEG and sleep apnea patterns is an exciting area of research that holds potential for improving identification and treatment. By comprehending how sleep apnea affects cerebral function, healthcare professionals can formulate more effective strategies to assist patients achieve better sleep and improve their overall health. As studies progresses to evolve, it is likely that qEEG will become an essential tool in the battle against sleep apnea, resulting to better outcomes for those who suffer from this difficult disorder.